Background: Thiotepa-based autologous stem cell transplantation (ASCT) improves survival in primary central nervous system lymphoma (PCNSL) but up to 30-60% of patients are unable to receive ASCT after MATRix induction, frequently due to treatment-related adverse events. Common conditioning regimens such as thiotepa/BCNU or thiotepa/busulfan/cyclophosphamide have also been associated with risks of pulmonary toxicity or increased transplant-related mortality. Novel strategies to improve the utilization and tolerability of ASCT are therefore needed to maximize the curative potential of this therapy in PCNSL.
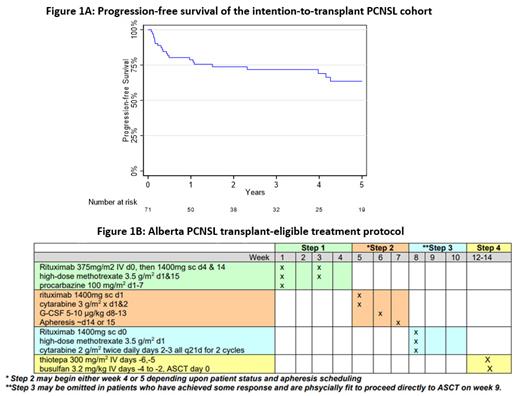
Methods: This retrospective population-based study included all patients diagnosed with large B-cell lymphoma-type PCNSL who were intended for ASCT in the province of Alberta, Canada between 2011 and 2022. Provincial treatment guidelines recommended an abbreviated, low-intensity induction protocol to reduce toxicity and increase transplantation rates (Figure 1B). Step 1 included 2 cycles of rituximab/high-dose methotrexate (HD-MTX). Step 2 involved 1 cycle of rituximab/high-dose cytarabine (HDAC) for peripheral blood stem cell mobilization. Step 3 consisted of 2 cycles of rituximab/HD-MTX/HDAC and was made optional in July 2018 so that patients with sufficient disease response and performance status following Step 2 could proceed immediately to ASCT. Conditioning consisted of thiotepa 300 mg/m 2 ×2 days and busulfan 3.2mg/kg ×3 days (TT/Bu). Dose reductions of TT/Bu by 10% for every 5 years over the age of 60 were recommended as of May 2021. Progression-free survival (PFS) and overall survival (OS) were determined using the Kaplan-Meier method and compared between groups using the log-rank test.
Results: The intention-to-transplant (ITT) cohort included 71 patients with median age 58 years (range 26-72), representing 81% of patients aged 18-60 and 55% of those aged 61-72 who were diagnosed with PCNSL in Alberta during the study period. The proportion of patients aged 61-72 who were treated with ITT increased from 42% before 2018 to 70% afterwards.
Fifty-six (79%) ITT patients proceeded to ASCT while 15 (21%) did not due to poor performance status (n=6), treatment-related adverse events (n=5), or disease progression (n=4). There was 1 (1%) death due to infection-related non-relapse mortality (NRM) during induction. The routine omission of Step 3 starting in 2018 resulted in high transplantation rates at 29/35 (83%) compared to 27/36 (75%) in the preceding era.
With median follow-up time 3.9 years, the 4-year PFS was 69% (95% CI 56-79%) and OS was 80% (95% CI 67-88%) in the ITT cohort (Figure 1A). For the 56 patients who received ASCT, 4-year PFS was 75% (95% CI 57-86%) and OS was 85% (95% CI 68-93%) from the time of ASCT. There was no significant difference in PFS between patients in complete response (CR)/unconfirmed CR versus partial response (PR) before ASCT (p=0.86); however, 5 patients with progressive disease before ASCT had inferior PFS compared to those with CR/CRu/PR (4-year PFS 40% vs 82%, p=0.0002). Relapse occurred in 8 (14%) patients at median 373 days (range 54-1411) after ASCT, including 7 with CNS relapse and 1 with systemic relapse. No patient in remission after ASCT received whole brain radiation therapy and most recovered without clinically significant neurologic deficits. There were no deaths due to transplant-related mortality. NRM occurred in 2 (4%) patients due to an unrelated cancer and stroke 1.1 and 4.3 years after ASCT, respectively.
Among 27 patients >60 years old treated with ITT, 17 (63%) proceeded to ASCT, including 6 who received dose reductions of TT/Bu. The transplantation rate in this age group increased from 45% to 75% following the routine omission of Step 3. All 17 transplanted patients remain alive and in remission with median follow-up 2.5 years.
Conclusion:In this real-world study of 71 patients with PCNSL, an abbreviated, low-intensity induction protocol resulted in high transplantation rates (~80%) and favorable long-term outcomes with 4-year OS 80%. Notably, TT/Bu conditioning achieved a low incidence of relapse with no transplant-related mortality observed, including among patients >60 years old. These data demonstrate that de-escalated induction therapy can result in improved rates of successful ASCT, thereby optimizing the outcomes of PCNSL.
Disclosures
Puckrin:Kite: Honoraria; Beigene: Honoraria; Incyte: Honoraria. Owen:F. Hoffmann-La Roche Ltd, AbbVie, Astrazeneca, Beigene, Merck, Incyte, Seattle Genetics, Novartis: Honoraria. Street:Seattle Genetics: Honoraria; Recordati: Honoraria; Kyowa Kirin: Honoraria. Perry:Beigene: Honoraria; Novartis: Honoraria; Seattle Genetics: Honoraria; Sobi: Honoraria; Incyte: Honoraria. Shafey:AstraZeneca: Honoraria; Roche: Honoraria. Stewart:Amgen: Honoraria; Celgene: Honoraria; Gilead: Honoraria; Sandoz: Honoraria; Janssen: Honoraria; Novartis: Honoraria; Abbvie: Honoraria; AstraZeneca: Honoraria; Roche: Honoraria; Teva: Honoraria.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal